Dr. Urmila Soman
As a gynecologist, I am intimately familiar with the intricate landscape of the female pelvis. It’s a densely packed anatomical region, a delicate ecosystem housing vital organs like the ovaries, uterus, fallopian tubes, bladder, and bowel, all supported by a complex network of ligaments. When surgical intervention becomes necessary in this confined space, the challenges are immense. Conditions such as ovarian abscesses, endometriosis, or uterine fibroids frequently demand surgical management, yet traditional approaches carry the inherent risk of collateral damage to healthy tissues – a concern that weighs heavily, particularly when future fertility is at stake.
Why Every Procedure Demands Fertility Preservation
The biological reality for women is that we are born with a finite reserve of oocytes; ovarian tissue, once lost, does not regenerate. This biological truth elevates fertility preservation from a desirable outcome to an absolute imperative, especially for younger women undergoing pelvic surgery. Consider the case of an ovarian abscess – a localized pocket of pus. While the primary goal of surgery is to eradicate the infection, conventional techniques, by their very nature, can inadvertently compromise or destroy healthy ovarian tissue nearby. This loss isn’t just about the immediate health of the ovary; it can profoundly impact a woman’s ability to conceive and even disrupt her delicate hormonal balance. This is precisely why the preservation of reproductive architecture through minimally invasive surgical procedures is not just a trend, but a critical evolution in our practice.
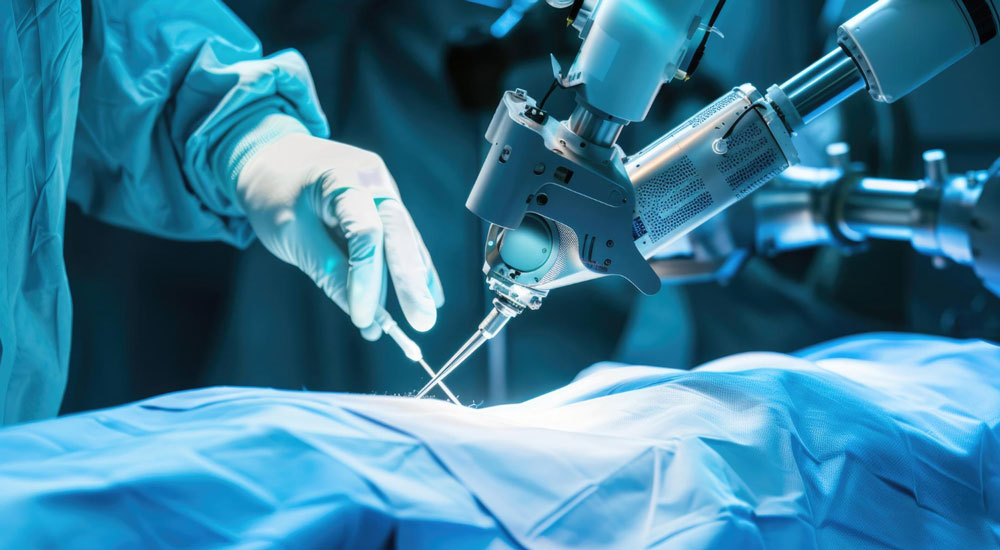
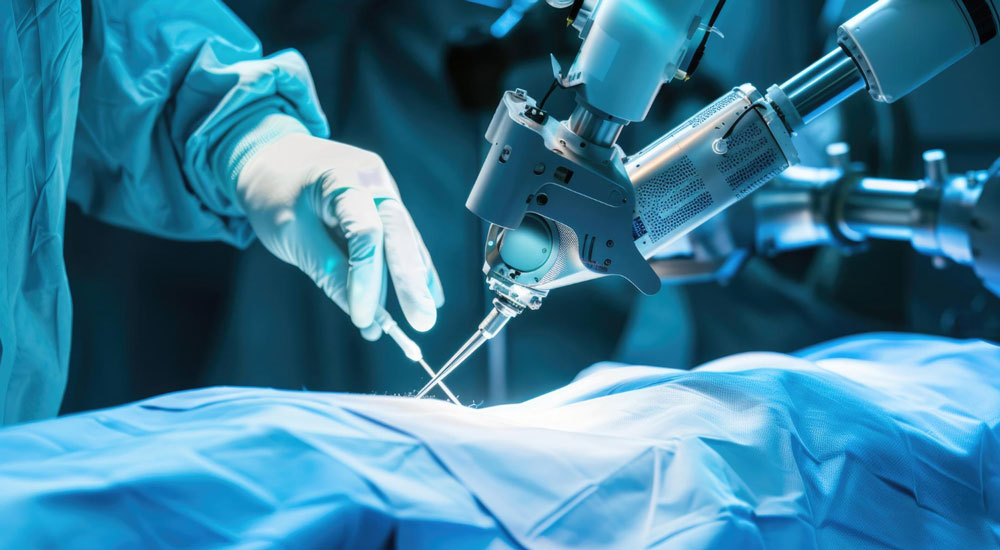
Robotic Surgery for Gynecological Precision
The advent of robotic-assisted surgery marks a pivotal moment in gynecological treatment. Systems like the da Vinci Surgical System offer a level of control and accuracy that simply wasn’t achievable with open surgery or even conventional laparoscopy. From a console, I can manipulate robotic arms, equipped with 3mm instruments that boast an astonishing 360-degree range of motion. What truly sets this technology apart is the visualization: a 10-fold magnification of the operative field, presenting a high-definition, three-dimensional view of the anatomical structures. This superior visualization allows for the discerning of fine tissue planes and structures that are often obscure during conventional laparoscopy. Beyond visual clarity, robotic systems enhance manual dexterity by filtering out tremors, ensuring remarkable accuracy in tissue manipulation and suturing, even during the most complex procedures.
Unlike the limitations of human fingers or traditional surgical instruments, robotic tools can navigate the small, intricate pelvic area with remarkable precision, minimizing trauma to surrounding healthy tissues. In gynecologic operations, where even the slightest injury to healthy tissue can have lasting consequences, this attribute is invaluable.
Targeting Ovarian Abscesses with Unparalleled Precision
Ovarian abscesses, often stemming from pelvic inflammatory disease or post-surgical infections, can rapidly become life-threatening if left untreated. Drainage or removal is essential, but the precision required to avoid harming healthy ovarian tissue is, as I’ve emphasized, paramount. Robotic surgery empowers us to precisely identify and excise only the abscessed tissue, safeguarding the ovary’s delicate structure and its vital function. The combination of 3D visualization and enhanced dexterity allows for optimal outcomes with a significantly reduced risk of complications.
Endometriosis: Unraveling Adhesions with Robotic Finesse
Endometriosis, a chronic condition where endometrial-like tissue grows outside the uterus, frequently leads to painful and debilitating adhesions. These fibrotic bands can cause organs, including the ovaries, bladder, and colon, to fuse together, distorting anatomy and impeding function. When addressing extensive pelvic adhesions in endometriosis, especially when fertility preservation is a primary concern, robotic-assisted surgery has become indispensable. The precision afforded by robotic tools is critical when operating near delicate structures like the fallopian tubes or the ovarian cortex. This meticulous approach allows us to minimize the decrease in Anti-Müllerian Hormone (AMH), a key indicator of ovarian reserve, and can even lower the rates of de novo adhesion formation, further contributing to the preservation of reproductive potential. Robotic surgery offers a highly precise method for excising endometriotic implants and carefully separating adhered organs. We can navigate between delicate tissue planes without causing undue trauma, significantly reducing the risk of organ damage or postoperative adhesion formation. This capability is paramount for patients who hope to maintain their reproductive potential. In challenging cases of deep-infiltrating endometriosis involving structures like the rectovaginal septum or uterosacral ligaments, robotic surgery facilitates precise dissection within narrow anatomical corridors, significantly enhancing both safety and the completeness of excision.




